Usuario:Facu89/Cesación tabáquica
Reducción gradual[editar]
La reducción gradual implica reducir el propio consumo de nicotina. En teoría, esto puede ser logrado a través de sucesivos cambios a cigarrilos con menores niveles de nicotina, reduciendo el número de cigarrilos por día, o fumando sólo una fracción de cada cigarrillo en cada ocasión. Una revisión sistemática de 2009 por investigadores de la Universidad de Birmingham encontró que la terapia de reemplazo nicotínico podría ser efectiva en la cesación tabáquica.[1][2] A 2010 Cochrane review found that abrupt cessation and gradual reduction with pre-quit NRT produced similar quit rates whether or not pharmacotherapy or psychological support was used. [3][4] According to a more recent 2012 Cochrane systematic review analysis of 10 studies and 3670 patients, overall relative risk reduction between smokers who attempted to quit with abrupt cessation or with gradual reduction techniques was 0.06. This analysis demonstrated that there was no significant difference in quit rates between smokers who quit by gradual reduction or abrupt cessation as measured by abstinence from smoking of at least six months from the quit day, suggesting that patients who want to quit can choose between these two methods.[5]
Community interventions[editar]
A Cochrane review found evidence that community interventions using "multiple channels to provide reinforcement, support and norms for not smoking" had an effect on smoking cessation outcomes among adults.[6] Specific methods used in the community to encourage smoking cessation among adults include:
- Policies making workplaces[7] and public places smoke-free. It is estimated that "comprehensive clean indoor laws" can increase smoking cessation rates by 12%–38%.[8] In 2008, the New York State of Alcoholism and Substantance Abuse Services banned smoking by patients, staff and volunteers at 1,300 addiction treatment centers.[9]
- Voluntary rules making homes smoke-free, which are thought to promote smoking cessation.[7][10]
- Initiatives to educate the public regarding the health effects of second-hand smoke.
- Increasing the price of tobacco products, for example by taxation. The US Task Force on Community Preventive Services found "strong scientific evidence" that this is effective in increasing tobacco use cessation.[11]: 28–30 It is estimated that an increase in price of 10% will increase smoking cessation rates by 3–5%.[8]
- Mass media campaigns. The US Task Force on Community Preventive Services declared that "strong scientific evidence" existed for these when "combined with other interventions"[11]: 30–32 , but a Cochrane review concluded that it was "difficult to establish their independent role and value".[12]
Competitions and incentives[editar]
One 2008 Cochrane review concluded that "incentives and competitions have not been shown to enhance long-term cessation rates."[13] However, a trial published in 2009 found that financial incentives for smoking cessation led to significantly higher rates of smoking cessation 15–18 months after enrollment.[14] Furthermore, a different 2008 Cochrane review found that one type of competition, "Quit and Win," did increase quit rates among participants.[15]
Psychosocial approaches[editar]
- Great American Smokeout is an annual event that invites smokers to quit for one day, hoping they will be able to extend this forever.
- The World Health Organization's World No Tobacco Day is held on May 31 each year.
- Smoking-cessation support is often offered over the internet, over the telephone quitlines[16][17] (e.g., the US toll-free number 1-800-QUIT-NOW), or in person. Three meta-analyses have concluded that telephone cessation support is effective when compared with minimal or no counselling or self-help, and that telephone cessation support with medication is more effective than medication alone.[18]: 91–92 [11]: 40–42 [19]
- Group or individual psychological support can help people who want to quit. This form of counselling can be effective alone; combining it with medication is more effective, and the number of sessions of support with medication correlates with effectiveness.[18]: 89–90, 101–103 [20][21] The counselling styles that have been effective in smoking cessation activities include motivational interviewing,[22][23][24] cognitive behavioural therapy[25] and Acceptance and Commitment Therapy.[26][26]
- The Freedom From Smoking group clinic includes eight sessions and features a step-by-step plan for quitting smoking. Each session is designed to help smokers gain control over their behavior. The clinic format encourages participants to work on the process and problems of quitting both individually and as part of a group[27]
- Multiple formats of psychosocial interventions increase quit rates: 10.8% for no intervention, 15.1% for one format, 18.5% for 2 formats, and 23.2% for three or four formats.[18]: 91
- The Transtheoretical Model including "stages of change" has been used in tailoring smoking cessation methods to individuals.[28][29][30][31] However, a 2010 Cochrane review concluded that "stage-based self-help interventions (expert systems and/or tailored materials) and individual counselling were neither more nor less effective than their non-stage-based equivalents."[32]
Self-help[editar]
A 2005 Cochrane review found that self-help materials may produce only a small increase in quit rates.[33] In the 2008 Guideline, "the effect of self-help was weak," and the number of types of self-help did not produce higher abstinence rates.[18]: 89–91 Nevertheless, self-help modalities for smoking cessation include:
- In-person self-help groups such as Nicotine Anonymous[34][35] or electronic self-help groups such as Stomp It Out.[36]
- Newsgroups: The Usenet group alt.support.stop-smoking has been used by people quitting smoking as a place to go to for support from others.[37] It is accessible through Google Groups.[38] and is now also available as an online forum, at http://www.as3-web.org/discuss .
- Interactive web-based and stand-alone computer programs and online communities which assist participants in quitting, such as EX and QuitNet. For example, "quit meters" keep track of statistics such as how long a person has remained abstinent.[39] In the 2008 US Guideline, there was no meta-analysis of computerised interventions, but they were described as "highly promising."[18]: 93–94 A meta-analysis published in 2009,[40] a Cochrane review published in 2010,[41] and a 2011 systematic review[42] found the evidence base for such interventions weak.
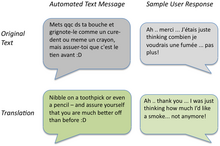
- Mobile phone-based interventions: A 2009 Cochrane review stated that "more evidence is needed" to determine the effectiveness of such interventions.[43] As of 2009, a randomised trial of mobile phone-based smoking cessation support was underway in the UK.[44]
- Self-help books such as Allen Carr's Easy Way to Stop Smoking.[45]
- Spirituality: In one survey of adult smokers, 88% reported a history of spiritual practice or belief, and of those more than three-quarters were of the opinion that using spiritual resources may help them quit smoking.[46]
Substitutes for cigarettes[editar]
- Electronic cigarette: Shaped like a cigarette to emulate the tactile experience of smoking, electronic cigarettes contain a rechargeable battery and a heating element which vaporises liquid nicotine and other flavorings from an insertable cartridge. Proponents of electronic cigarettes often market them as a smoking cessation device. Many claim that electronic cigarettes deliver the experience of smoking without the adverse health effects usually associated with tobacco smoke, or at least greatly reduce those risks.[47] However, in September 2008, the World Health Organization issued a release proclaiming that it does not consider the electronic cigarette to be a legitimate smoking cessation aid, stating that "no rigorous, peer-reviewed studies have been conducted showing that the electronic cigarette is a safe and effective nicotine replacement therapy."[48]
- The US National Institute of Health recommends chewing cinnamon sticks when trying to quit the use of tobacco. In addition to raw cinnamon sticks, cinnamon-flavoured toothpicks are used to help curb the urge for tobacco.[49][50]
- Plastic cigarette substitute: In one 2006 study, giving people a free "Better Quit" hollow tube resembling a cigarette did not improve quit rates.[51]
Alternative approaches[editar]
- Acupuncture: Acupuncture has been explored as an adjunct treatment method for smoking cessation.[52] A Cochrane review concluded that acupuncture "do[es] not appear to help smokers who are trying to quit",[53] a meta-analysis from the 2008 Guideline showed no difference between acupuncture and placebo,[18]: 99–100 and the 2008 Guideline found no scientific studies supporting laser therapy based on acupuncture principles but without the needles.[18]: 99
- Aromatherapy: A 2006 book reviewing the scientific literature on aromatherapy[54] identified only one study on smoking cessation and aromatherapy; the study found that "inhalation of vapor from black pepper extract reduces smoking withdrawal symptoms".[55]
- Hypnosis: Hypnosis often involves the hypnotherapist suggesting to the patient the unpleasant outcomes of smoking.[56] Clinical trials studying hypnosis and hypnotherapy as a method for smoking cessation have been inconclusive[18]: 100 ;[57][58][59] however, a randomized trial published in 2008 found that hypnosis and nicotine patches "compares favorably" with standard behavioral counseling and nicotine patches in 12-month quit rates.[60]
- Herbs: Many herbs have been studied as a method for smoking cessation, including lobelia and St John's wort.[61][62] The results are inconclusive, but St. Johns Wort shows few adverse events. Lobelia has been used to treat respiratory diseases like asthma and bronchitis, and has been used for smoking cessation because of chemical similarities to tobacco; lobelia is now listed in the FDA's Poisonous Plant Database.[63][64] Lobelia can still be found in many products sold for smoking cessation and should be used with caution.
- Smokeless tobacco: There is little smoking in Sweden, which is reflected in the very low cancer rates for Swedish men. Use of snus (a form of steam-pasteurised, rather than heat-pasteurised, air-cured smokeless tobacco) is an observed cessation method for Swedish men and even recommended by some Swedish doctors.[65]
- There are many other measures used in an effort to quit smoking which lack evidence including: a substance put on the cigarette called NicoBloc.[66] Due to the lack of evidence they are typically not recommended.[67]
Special populations[editar]
Children and adolescents[editar]
Methods used with children and adolescents include:
- Motivational enhancement[68]
- Psychological support[68]
- Youth anti-tobacco activities, such as sport involvement
- School-based curricula, such as life-skills training
- School-based nurse counseling sessions[69]
- Access reduction to tobacco
- Anti-tobacco media
- Family communication
A Cochrane review, mainly of studies combining motivational enhancement and psychological support, concluded that "complex approaches" for smoking cessation among young people show promise.[68] The 2008 US Guideline recommends counselling-style support for adolescent smokers on the basis of a meta-analysis of seven studies.[18]: 159–161 Neither the Cochrane review nor the 2008 Guideline recommends medications for adolescents who smoke.
Pregnant women[editar]
Smoking during pregnancy can cause adverse health effects in both the woman and the fetus. The 2008 US Guideline determined that "person-to-person psychosocial interventions" (typically including "intensive counseling") increased abstinence rates in pregnant women who smoke to 13.3%, compared with 7.6% in usual care.[18]: 165–167 Mothers who smoke during pregnancy have a greater tendency towards premature births. Their babies are often underdeveloped, have smaller organs, and weigh much less compared with the normal baby. In addition, these babies have worse immune systems, making them more susceptible to many diseases in early childhood, such as middle ear inflammations and asthmatic bronchitis which can bring about a lot of agony and suffering. As well, there is a high chance that they will become smokers themselves when grown up.
It is a widely spread myth that a female smoker can cause harm to her fetus by quitting immediately upon discovering that she is with child. Though this idea does seem to follow logic, it is not based on any medical study or fact.[70]
Workers[editar]
A 2008 Cochrane review of smoking cessation activities in work-places concluded that "interventions directed towards individual smokers increase the likelihood of quitting smoking."[71] A 2010 systematic review determined that worksite incentives and competitions needed to be combined with additional interventions to produce significant increases in smoking cessation rates.[72]
Hospitalised smokers[editar]
Smokers who are hospitalised may be particularly motivated to quit.[18]: 149–150 A 2007 Cochrane review found that interventions beginning during a hospital stay and continuing for one month or more after discharge were effective in producing abstinence.[74] But the use of Swedish snus should be considered for use by patients who require not only the nicotine but the other alkaloids present in tobacco that users enjoy.
Comparison of success rates[editar]
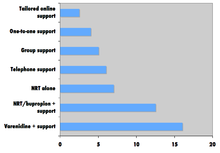
Comparison of success rates across interventions can be difficult because of different definitions of "success" across studies.[75] Robert West and Saul Shiffman, authorities in this field recognised by government health departments in a number of countries [73]: 73, 76, 80 , have concluded that, used together, "behavioural support" and "medication" can quadruple the chances that a quit attempt will be successful.
A 2008 systematic review in the European Journal of Cancer Prevention found that group behavioural therapy was the most effective intervention strategy for smoking cessation, followed by bupropion, intensive physician advice, nicotine replacement therapy, individual counselling, telephone counselling, nursing interventions, and tailored self-help interventions; the study did not discuss varenicline.[8]

Factors affecting success[editar]
Quitting can be harder for individuals with dark pigmented skin compared to individuals with pale skin since nicotine has an affinity for melanin-containing tissues. Studies suggest this can cause the phenomenon of increased nicotine dependence and lower smoking cessation rate in darker pigmented individuals.[77]
There is an important social component to smoking. A 2008 study of a densely interconnected network of over 12,000 individuals found that smoking cessation by any given individual reduced the chances of others around them lighting up by the following amounts: a spouse by 67%, a sibling by 25%, a friend by 36%, and a coworker by 34%.[78] Nevertheless, a Cochrane review determined that interventions to increase social support for a smoker's cessation attempt did not increase long-term quit rates.[79]
Smokers who are trying to quit are faced with social influences that may persuade them to conform and continue smoking. Cravings are easier to detain when ones environment does not provoke the habit. If a person who stopped smoking has close relationships with active smokers they are often put into situations that make the urge to conform more tempting. However, in a small group with at least one other not smoking, the likelihood of conformity decreases. The social influence to smoke cigarettes has been proven to rely on simple variables. One researched variable depends on whether the influence is from a friend or non-friend.[80] the research shows that individuals are 77% more likely to conform to non-friends, while close friendships decrease conformity. Therefore, if an acquaintance offers a cigarette as a polite gesture, the person who has stopped smoking will be more likely to break his commitment than if a friend had offered.
Smokers with major depressive disorder may be less successful at quitting smoking than non-depressed smokers.[18]: 81 [81]
Relapse (resuming smoking after quitting) has been related to psychological issues such as low self-efficacy[82] or non-optimal coping responses;[83] however, psychological approaches to prevent relapse have not been proven to be successful.[84] In contrast, varenicline may help some relapsed smokers.[84]
Side effects[editar]
| Craving for tobacco | 3 to 8 weeks[85] |
| Dizziness | Few days[85] |
| Insomnia | 1 to 2 weeks[85] |
| Headaches | 1 to 2 weeks[85] |
| Chest discomfort | 1 to 2 weeks[85] |
| Constipation | 1 to 2 weeks[85] |
| Irritability | 2 to 4 weeks[85] |
| Fatigue | 2 to 4 weeks[85] |
| Cough or nasal drip | Few weeks[85] |
| Lack of concentration | Few weeks[85] |
| Hunger | Up to several weeks[85] |
Symptoms[editar]
In a 2007 review of the effects of abstinence from tobacco, Hughes concluded that "anger, anxiety, depression, difficulty concentrating, impatience, insomnia, and restlessness are valid withdrawal symptoms that peak within the first week and last 2–4 weeks."[86] In contrast, "constipation, cough, dizziness, increased dreaming, and mouth ulcers" may or may not be symptoms of withdrawal, while drowsiness, fatigue, and certain physical symptoms ("dry mouth, flu symptoms, headaches, heart racing, skin rash, sweating, tremor") were not symptoms of withdrawal.[86]
Weight gain[editar]
Giving up smoking is associated with an average weight gain of 4-5 kilogramos (8,8-11,0 lb) after 12 months, most of which occurs within the first three months of quitting.[87]
The possible causes of the weight gain include:
- Smoking over-expresses the gene AZGP1 which stimulates lipolysis, so smoking cessation may decrease lipolysis.[88]
- Smoking suppresses appetite, which may be caused by nicotine's effect on central autonomic neurons (e.g., via regulation of melanin concentrating hormone neurons in the hypothalamus).[89]
- Heavy smokers are reported to burn 200 calories per day more than non-smokers eating the same diet.[90] Possible reasons for this phenomenon include nicotine's ability to increase energy metabolism or nicotine's effect on peripheral neurons.[89]
The 2008 Guideline suggests that sustained-release bupropion, nicotine gum, and nicotine lozenge be used "to delay weight gain after quitting."[18]: 173–176 However, a 2012 Cochrane review concluded that "The data are not sufficient to make strong clinical recommendations for effective programmes" for preventing weight gain.[91]
Depression[editar]
Like other physically addictive drugs, nicotine withdrawal causes down-regulation of the production of dopamine and other stimulatory neurotransmitters as the brain attempts to compensate for artificial stimulation. Therefore, when people stop smoking, depressive symptoms such as suicidal tendencies or actual depression may result.[81][92] This side effect of smoking cessation may be particularly common in women, as depression is more common among women than among men.[93]
Anxiety[editar]
A recent study by The British Journal of Psychiatry has found that smokers who successfully quit feel less anxious afterwards with the effect being greater among those who had mood and anxiety disorders than those that smoked for pleasure.[94]
Health benefits[editar]
Many of tobacco's detrimental health effects can be reduced or largely removed through smoking cessation. The health benefits over time of stopping smoking include:[95]
- Within 20 minutes after quitting, blood pressure and heart rate decrease
- Within 12 hours, carbon monoxide levels in the blood decrease to normal
- Within 48 hours, nerve endings and sense of smell and taste both start recovering
- Within 3 months, circulation and lung function improve
- Within 9 months, there are decreases in cough and shortness of breath
- Within 1 year, the risk of coronary heart disease is cut in half
- Within 5 years, the risk of stroke falls to the same as a non-smoker, and the risks of many cancers (mouth, throat, esophagus, bladder, cervix) decrease significantly
- Within 10 years, the risk of dying from lung cancer is cut in half,[96] and the risks of larynx and pancreas cancers decrease
- Within 15 years, the risk of coronary heart disease drops to the level of a non-smoker; lowered risk for developing COPD (chronic obstructive pulmonary disease)
The British doctors study showed that those who stopped smoking before they reached 30 years of age lived almost as long as those who never smoked.[97] Stopping in one's sixties can still add three years of healthy life.[97] A randomized trial from the U.S. and Canada showed that a smoking cessation program lasting 10 weeks decreased mortality from all causes over 14 years later.[98]
Another published study, "Smoking Cessation Reduces Postoperative Complications: A Systematic Review and Meta-analysis," examined six randomized trials and 15 observational studies to look at the effects of preoperative smoking cessation on postoperative complications. The findings were: 1) taken together, the studies demonstrated decreased likelihood of postoperative complications in patients who ceased smoking prior to surgery; 2) overall, each week of cessation prior to surgery increased the magnitude of the effect by 19%. A significant positive effect was noted in trials where smoking cessation occurred at least four weeks prior to surgery; 3) For the six randomized trials, they demonstrated on average a relative risk reduction of 41% for postoperative complications.[99]
Cost-effectiveness[editar]

Cost-effectiveness analyses of smoking cessation activities have shown that they increase quality-adjusted life years (QALYs) at costs comparable with other types of interventions to treat and prevent disease.[18]: 134–137 Studies of the cost-effectiveness of smoking cessation include:
- In a 1997 U.S. analysis, the estimated cost per QALY varied by the type of cessation approach, ranging from group intensive counselling without nicotine replacement at $1108 per QALY to minimal counselling with nicotine gum at $4542 per QALY.[100]
- A study from Erasmus University Rotterdam limited to people with chronic obstructive pulmonary disease found that the cost-effectiveness of minimal counselling, intensive counselling, and drug therapy were €16,900, €8,200, and €2,400 per QALY gained respectively.[101]
- Among National Health Service smoking cessation clients in Glasgow, pharmacy one-to-one counselling cost £2,600 per QALY gained and group support cost £4,800 per QALY gained.[102]
Statistical trends[editar]
The frequency of smoking cessation among smokers varies across countries. Smoking cessation increased in Spain between 1965 and 2000,[103] in Scotland between 1998 and 2007,[104] and in Italy after 2000.[105] In contrast, in the U.S. the cessation rate was "stable (or varied little)" between 1998 and 2008,[106] and in China smoking cessation rates declined between 1998 and 2003.[107]
Nevertheless, in a growing number of countries there are now more ex-smokers than smokers.[108] For example, in the U.S. as of 2010, there were 47 million ex-smokers and 46 million smokers.[109]
See also[editar]
Referencias[editar]
- ↑ Phend C (3 de abril de 2009). «Gradual cutback with nicotine replacement boosts quit rates». MedPage Today. Consultado el 20 de febrero de 2011.
- ↑ Moore D, Aveyard P, Connock M, Wang D, Fry-Smith A, Barton P (2009). «Effectiveness and safety of nicotine replacement therapy assisted reduction to stop smoking: systematic review and meta-analysis». BMJ 338: b1024. PMC 2664870. PMID 19342408. doi:10.1136/bmj.b1024.
- ↑ Joseph J (March 30, 2010). «Cut down to quit approach no better». Pharmacy News (Reed Business Information).
- ↑ Lindson N, Aveyard P, Hughes JR (2010). «Reduction versus abrupt cessation in smokers who want to quit». En Lindson, Nicola, ed. Cochrane Database Syst Rev 3 (3): CD008033. PMID 20238361. doi:10.1002/14651858.CD008033.pub2.
- ↑ Lindson-Hawley N, Aveyard P, Hughes JR (2012). «Reduction versus abrupt cessation in smokers who want to quit». En Lindson-Hawley, Nicola, ed. Cochrane Database of Systematic Reviews 11 (11): CD008033. PMID 23152252. doi:10.1002/14651858.CD008033.pub3.
- ↑ Secker-Walker RH, Gnich W, Platt S, Lancaster T (2002). «Community interventions for reducing smoking among adults». En Stead, Lindsay F, ed. Cochrane Database Syst Rev (3): CD001745. PMID 12137631. doi:10.1002/14651858.CD001745.
- ↑ a b Error en la cita: Etiqueta
<ref>no válida; no se ha definido el contenido de las referencias llamadasLee2007 - ↑ a b c Lemmens V, Oenema A, Knut IK, Brug J (2008). «Effectiveness of smoking cessation interventions among adults: a systematic review of reviews». Eur J Cancer Prev 17 (6): 535-44. PMID 18941375. doi:10.1097/CEJ.0b013e3282f75e48.
- ↑ «State-Mandated Tobacco Ban, Integration of Cessation Services, and Other Policies Reduce Smoking Among Patients and Staff at Substance Abuse Treatment Centers». Agency for Healthcare Research and Quality. 27 de febrero de 2013. Consultado el 13 de mayo de 2013.
- ↑ Centers for Disease Control and Prevention (CDC) (May 2007). «State-specific prevalence of smoke-free home rules--United States, 1992-2003». MMWR Morb. Mortal. Wkly. Rep. 56 (20): 501-4. PMID 17522588.
- ↑ a b c Error en la cita: Etiqueta
<ref>no válida; no se ha definido el contenido de las referencias llamadasHopkins2001 - ↑ Bala M, Strzeszynski L, Cahill K (2008). «Mass media interventions for smoking cessation in adults». En Bala, Malgorzata, ed. Cochrane Database Syst Rev (1): CD004704. PMID 18254058. doi:10.1002/14651858.CD004704.pub2.
- ↑ Cahill K, Perera R (2008). «Competitions and incentives for smoking cessation». En Cahill, Kate, ed. Cochrane Database Syst Rev (3): CD004307. PMID 18646105. doi:10.1002/14651858.CD004307.pub3.
- ↑ Volpp KG, Troxel AB, Pauly MV, Glick HA, Puig A, Asch DA, Galvin R, Zhu J, Wan F, DeGuzman J, Corbett E, Weiner J, Audrain-McGovern J (2009). «A randomized, controlled trial of financial incentives for smoking cessation». N Engl J Med 360 (7): 699-709. PMID 19213683. doi:10.1056/NEJMsa0806819.
- ↑ Cahill K, Perera R (2008). «Quit and Win contests for smoking cessation». En Cahill, Kate, ed. Cochrane Database Syst Rev (4): CD004986. PMID 18843674. doi:10.1002/14651858.CD004986.pub3.
- ↑ Zhu SH, Anderson CM, Tedeschi GJ, Rosbrook B, Johnson CE, Byrd M, Gutiérrez-Terrell E (2002). «Evidence of real-world effectiveness of a telephone quitline for smokers». N Engl J Med 347 (14): 1087-93. PMID 12362011. doi:10.1056/NEJMsa020660.
- ↑ Helgason AR, Tomson T, Lund KE, Galanti R, Ahnve S, Gilljam H (2004). «Factors related to abstinence in a telephone helpline for smoking cessation». Eur J Public Health 14 (3): 306-10. PMID 15369039. doi:10.1093/eurpub/14.3.306.
- ↑ a b c d e f g h i j k l m n Error en la cita: Etiqueta
<ref>no válida; no se ha definido el contenido de las referencias llamadasUSDHHS2008 - ↑ Stead LF, Perera R, Lancaster T (2006). «Telephone counselling for smoking cessation». En Stead, Lindsay F, ed. Cochrane Database Syst Rev 3 (3): CD002850. PMID 16855992. doi:10.1002/14651858.CD002850.pub2.
- ↑ Stead LF, Lancaster T (2005). «Group behaviour therapy programmes for smoking cessation». En Stead, Lindsay F, ed. Cochrane Database Syst Rev (2): CD001007. PMID 15846610. doi:10.1002/14651858.CD001007.pub2.
- ↑ Lancaster T, Stead LF (2005). «Individual behavioural counselling for smoking cessation». En Lancaster, Tim, ed. Cochrane Database Syst Rev (2): CD001292. PMID 15846616. doi:10.1002/14651858.CD001292.pub2.
- ↑ Lai DT, Cahill K, Qin Y, Tang JL (2010). «Motivational interviewing for smoking cessation». En Lai, Douglas TC, ed. Cochrane Database Syst Rev (1): CD006936. PMID 20091612. doi:10.1002/14651858.CD006936.pub2.
- ↑ Hettema JE, Hendricks PS (2010). «Motivational interviewing for smoking cessation: a meta-analytic review». J Consult Clin Psychol 78 (6): 868-84. PMID 21114344. doi:10.1037/a0021498.
- ↑ Heckman CJ, Egleston BL, Hofmann MT (2010). «Efficacy of motivational interviewing for smoking cessation: a systematic review and meta-analysis». Tob Control 19 (5): 410-6. PMC 2947553. PMID 20675688. doi:10.1136/tc.2009.033175.
- ↑ Perkins KA, Conklin CA, Levine MD (2008). Cognitive-behavioral therapy for smoking cessation: a practical guidebook to the most effective treatment. New York: Routledge. ISBN 978-0-415-95463-1.
- ↑ a b Ruiz, F. J. (2010). «A review of Acceptance and Commitment Therapy (ACT) empirical evidence: Correlational, experimental psychopathology, component and outcome studies». International Journal of Psychology and Psychological Therapy 10 (1): 125-62.
- ↑ http://www.lung.org/stop-smoking/how-to-quit/freedom-from-smoking/
- ↑ Prochaska JO, Velicer WF, DiClemente CC, Fava J (1988). «Measuring processes of change: applications to the cessation of smoking». J Consult Clin Psychol 56 (4): 520-8. PMID 3198809. doi:10.1037/0022-006X.56.4.520.
- ↑ DiClemente CC, Prochaska JO, Fairhurst SK, Velicer WF, Velasquez MM, Rossi JS (1991). «The process of smoking cessation: an analysis of precontemplation, contemplation, and preparation stages of change». J Consult Clin Psychol 59 (2): 295-304. PMID 2030191. doi:10.1037/0022-006X.59.2.295. Consultado el 15 de febrero de 2011.
- ↑ Velicer WF, Prochaska JO, Rossi JS, Snow MG (1992). «Assessing outcome in smoking cessation studies». Psychol Bull 111 (1): 23-41. PMID 1539088. doi:10.1037/0033-2909.111.1.23.
- ↑ Prochaska JO, DiClemente CC, Velicer WF, Rossi JS (1993). «Standardized, individualized, interactive, and personalized self-help programs for smoking cessation». Health Psychol 12 (5): 399-405. PMID 8223364. doi:10.1037/0278-6133.12.5.399. Consultado el 15 de febrero de 2011.
- ↑ Cahill K, Lancaster T, Green N (2010). «Stage-based interventions for smoking cessation». En Cahill, Kate, ed. Cochrane Database Syst Rev (11): CD004492. PMID 21069681. doi:10.1002/14651858.CD004492.pub4.
- ↑ Lancaster T, Stead LF (2005). «Self-help interventions for smoking cessation». En Lancaster, Tim, ed. Cochrane Database Syst Rev (3): CD001118. PMID 16034855. doi:10.1002/14651858.CD001118.pub2.
- ↑ «Nicotine Anonymous (official website)». Dallas, TX: Nicotine Anonymous World Services. Consultado el 21 de febrero de 2011.
- ↑ Glasser I (2010). «Nicotine Anonymous may benefit nicotine-dependent individuals». Am J Public Health 100 (2): 196; author reply 196-7. PMC 2804638. PMID 20019295. doi:10.2105/AJPH.2009.181545.
- ↑ «Stomp It Out». San Francisco, CA: Experience Project. Consultado el 21 de febrero de 2011.
- ↑ Uhler D (15 de noviembre de 1995). «Breaking the habit - these tips can keep your good intentions from going up in smoke». San Antonio Express-News.
- ↑ Google Groups. «alt.support.stop-smoking». Consultado el 21 de febrero de 2011.
- ↑ Hendrick B (26 de mayo de 2009). «Computer is an ally in quit-smoking fight. Study shows web- and computer-based programs help smokers quit». WebMD Health News. Consultado el 21 de febrero de 2011.
- ↑ Myung SK, McDonnell DD, Kazinets G, Seo HG, Moskowitz JM (2009). «Effects of Web- and computer-based smoking cessation programs: meta-analysis of randomized controlled trials». Arch Intern Med 169 (10): 929-37. PMID 19468084. doi:10.1001/archinternmed.2009.109.
- ↑ Civljak M, Sheikh A, Stead LF, Car J (2010). «Internet-based interventions for smoking cessation». En Car, Josip, ed. Cochrane Database Syst Rev (9): CD007078. PMID 20824856. doi:10.1002/14651858.CD007078.pub3.
- ↑ Hutton HE, Wilson LM, Apelberg BJ, Avila Tang E, Odelola O, Bass EB, Chander G (Feb 2011). «A systematic review of randomized controlled trials: web-based interventions for smoking cessation among adolescents, college students, and adults». Nicotine Tob Res 13 (4): 227-38. PMID 21350042. doi:10.1093/ntr/ntq252.
- ↑ Whittaker R, Borland R, Bullen C, Lin RB, McRobbie H, Rodgers A (2009). «Mobile phone-based interventions for smoking cessation». En Whittaker, Robyn, ed. Cochrane Database Syst Rev (4): CD006611. PMID 19821377. doi:10.1002/14651858.CD006611.pub2.
- ↑ Free C, Whittaker R, Knight R, Abramsky T, Rodgers A, Roberts IG (2009). «Txt2stop: a pilot randomised controlled trial of mobile phone-based smoking cessation support». Tob Control 18 (2): 88-91. PMID 19318534. doi:10.1136/tc.2008.026146.
- ↑ Error en la cita: Etiqueta
<ref>no válida; no se ha definido el contenido de las referencias llamadasCarr2004 - ↑ Gonzales D, Redtomahawk D, Pizacani B, Bjornson WG, Spradley J, Allen E, Lees P (2007). «Support for spirituality in smoking cessation: results of pilot survey». Nicotine Tob Res 9 (2): 299-303. PMID 17365761. doi:10.1080/14622200601078582.
- ↑ «E-Cigarette – An Excellent Subsitute to Tobacco Cigarettes». AbsolutelyeCigs.com. 25 January 2012. Consultado el 9 de mayo de 2012.
- ↑ «Marketers of electronic cigarettes should halt unproved therapy claims». World Health Organization. 19 de septiembre de 2008. Consultado el 21 de febrero de 2011.
- ↑ «Smoking - tips on how to quit». Nlm.nih.gov. 27 de julio de 2012. Consultado el 5 de agosto de 2012.
- ↑ «Cinnamon Curbs the Urge and More». Candycrate.com. Consultado el 5 de agosto de 2012.
- ↑ Bauer JE, Carlin-Menter SM, Celestino PB, Hyland A, Cummings KM (2006). «Giving away free nicotine medications and a cigarette substitute (Better Quit) to promote calls to a quitline». J Public Health Manag Pract 12 (1): 60-7. PMID 16340517. doi:10.1097/00124784-200601000-00012.
- ↑ He, Dong; Berg, John E.; Høstmark, Arne T. (March 1997). «Effects of acupuncture on smoking cessation or reduction for motivated smokers». Preventive Medicine 26 (2): 208-214. PMID 9085389. doi:10.1006/pmed.1996.0125.
- ↑ White AR, Rampes H, Liu JP, Stead LF, Campbell J (2011). «Acupuncture and related interventions for smoking cessation». En White, Adrian R, ed. Cochrane Database Syst Rev (1): CD000009. PMID 21249644. doi:10.1002/14651858.CD000009.pub3.
- ↑ Lis-Balchin M (2006). Aromatherapy science: a guide for healthcare professionals. London: Pharmaceutical Press. p. 101. ISBN 0-85369-578-4.
- ↑ Rose JE, Behm FM (1994). «Inhalation of vapor from black pepper extract reduces smoking withdrawal symptoms». Drug Alcohol Depend 34 (3): 225-9. PMID 8033760. doi:10.1016/0376-8716(94)90160-0.
- ↑ «Hypnosis for Quitting Smoking». WebMD. Consultado el 19 de mayo de 2012.
- ↑ Barnes J, Dong CY, McRobbie H, Walker N, Mehta M, Stead LF (2010). «Hypnotherapy for smoking cessation». En Barnes, Jo, ed. Cochrane Database Syst Rev (10): CD001008. PMID 20927723. doi:10.1002/14651858.CD001008.pub2.
- ↑ Johnson, D.L.; Karkut, R.T. (October 1994). «Performance by gender in a stop-smoking program combining hypnosis and aversion». Psychological reports 75 (2): 851-7. PMID 7862796. doi:10.2466/pr0.1994.75.2.851.
- ↑ Law, Malcolm; Tang, Jin Ling (1995). «An analysis of the effectiveness of interventions intended to help people stop smoking». Arch Intern Med. 155 (18): 1933-1941. PMID 7575046. doi:10.1001/archinte.1995.00430180025004.
- ↑ Carmody TP, Duncan C, Simon JA, Solkowitz S, Huggins J, Lee S, Delucchi K (2008). «Hypnosis for smoking cessation: a randomized trial». Nicotine Tob Res 10 (5): 811-8. PMID 18569754. doi:10.1080/14622200802023833.
- ↑ Mayo Clinic. St. John's Wort for Tobacco Cessation.
- ↑ Mayo, Clinic. «St. John's Wort for Tobacco Cessation». US National Institute of Health. Consultado el 29 November 2006.
- ↑ FDA. FDA Poisonous Plant Database.
- ↑ FDA. «FDA Poisonous Plant Database». U.S. Food and Drug Administration. Consultado el 1 January 2008.
- ↑ SCENIHR, Health Effects of Smokeless Tobacco Products, p. 103.
- ↑ http://colinmendelsohn.com.au/files/9513/7031/1653/Mendelsohn_C._NIcotine_dependence._Australian_Doctor_How_to_Treat._June_2013.pdf
- ↑ McRobbie, H; Bullen, C; Glover, M; Whittaker, R; Wallace-Bell, M; Fraser, T; New Zealand Guidelines, Group (20 de junio de 2008). «New Zealand smoking cessation guidelines». The New Zealand medical journal 121 (1276): 57-70. PMID 18574510.
- ↑ a b c Grimshaw GM, Stanton A (2006). «Tobacco cessation interventions for young people». En Grimshaw, Gill, ed. Cochrane Database Syst Rev (4): CD003289. PMID 17054164. doi:10.1002/14651858.CD003289.pub4.
- ↑ «Intensive Counseling of Students by School Nurses Does Not Have Larger Impact on Long-Term Smoking Rates Than Briefer Sessions». Agency for Healthcare Research and Quality. 15 de mayo de 2013. Consultado el 10 de julio de 2013.
- ↑ Philip, Owen. «Pregnancy and Smoking». Net Doctor. Consultado el 9 April 2012.
- ↑ Cahill K, Moher M, Lancaster T (2008). «Workplace interventions for smoking cessation». En Cahill, Kate, ed. Cochrane Database Syst Rev (4): CD003440. PMID 18843645. doi:10.1002/14651858.CD003440.pub3.
- ↑ Leeks KD, Hopkins DP, Soler RE, Aten A, Chattopadhyay SK; Task Force on Community Preventive Services (2010). «Worksite-based incentives and competitions to reduce tobacco use. A systematic review». Am J Prev Med 38 (2 Suppl): S263-74. PMID 20117611. doi:10.1016/j.amepre.2009.10.034.
- ↑ a b Error en la cita: Etiqueta
<ref>no válida; no se ha definido el contenido de las referencias llamadasWestShiffman2007 - ↑ Rigotti NA, Munafo MR, Stead LF (2007). «Interventions for smoking cessation in hospitalised patients». En Rigotti, Nancy, ed. Cochrane Database Syst Rev (3): CD001837. PMID 17636688. doi:10.1002/14651858.CD001837.pub2.
- ↑ Error en la cita: Etiqueta
<ref>no válida; no se ha definido el contenido de las referencias llamadasACS-success - ↑ Naqvi NH, Rudrauf D, Damasio H, Bechara A (2007). «Damage to the insula disrupts addiction to cigarette smoking». Science 315 (5811): 531-4. PMC 3698854. PMID 17255515. doi:10.1126/science.1135926.
- ↑ King G, Yerger VB, Whembolua GL, Bendel RB, Kittles R, Moolchan ET (2009). «Link between facultative melanin and tobacco use among African Americans». Pharmacol Biochem Behav 92 (4): 589-96. PMID 19268687. doi:10.1016/j.pbb.2009.02.011.
- ↑ Christakis NA, Fowler JH (2008). «The collective dynamics of smoking in a large social network». N Engl J Med 358 (21): 2249-58. PMC 2822344. PMID 18499567. doi:10.1056/NEJMsa0706154.
- ↑ Park EW, Schultz JK, Tudiver F, Campbell T, Becker L (2004). «Enhancing partner support to improve smoking cessation». En Park, Eal Whan, ed. Cochrane Database Syst Rev (3): CD002928. PMID 15266469. doi:10.1002/14651858.CD002928.pub2.
- ↑ Peoples, Clayton D.; Sigillo, Alexandra E.; Green, Morgan; Miller, Monica K. (2012). «Friendship and Conformity in Group Opinions: Juror Verdict Change in Mock Juries». Sociological Spectrum 32 (2): 178. doi:10.1080/02732173.2012.646163.
- ↑ a b Glassman AH, Helzer JE, Covey LS, Cottler LB, Stetner F, Tipp JE, Johnson J (1990). «Smoking, smoking cessation, and major depression». JAMA 264 (12): 1546-9. PMID 2395194. doi:10.1001/jama.1990.03450120058029.
- ↑ Condiotte MM, Lichtenstein E (1981). «Self-efficacy and relapse in smoking cessation programs». J Consult Clin Psychol 49 (5): 648-58. PMID 7287974. doi:10.1037/0022-006X.49.5.648.
- ↑ Shiffman S (1982). «Relapse following smoking cessation: a situational analysis». J Consult Clin Psychol 50 (1): 71-86. PMID 7056922. doi:10.1037/0022-006X.50.1.71.
- ↑ a b Hajek P, Stead LF, West R, Jarvis M, Lancaster T (2009). «Relapse prevention interventions for smoking cessation». En Stead, Lindsay F, ed. Cochrane Database Syst Rev (1): CD003999. PMID 19160228. doi:10.1002/14651858.CD003999.pub3.
- ↑ a b c d e f g h i j k Kaiser Foundation Health Plan of the Northwest (2008). Cultivating Health: Freedom From Tobacco Kit. Kaiser Permanente. ISBN 978-0-9744864-8-2.[página requerida]
- ↑ a b Hughes JR (2007). «Effects of abstinence from tobacco: valid symptoms and time course». Nicotine Tob Res 9 (3): 315-27. PMID 17365764. doi:10.1080/14622200701188919.
- ↑ H.-J. Aubin, A. Farley, D. Lycett, P. Lahmek, P. Aveyard. (2012). «Weight gain in smokers after quitting cigarettes: meta-analysis». BMJ-British Medical Journal 345 (345): e4439. doi:10.1136/bmj.e4439.
- ↑ Vanni H, Kazeros A, Wang R, Harvey BG, Ferris B, De BP, Carolan BJ, Hübner RH, O'Connor TP, Crystal RG (2009). «Cigarette smoking induces overexpression of a fat-depleting gene AZGP1 in the human». Chest 135 (5): 1197-208. PMC 2679098. PMID 19188554. doi:10.1378/chest.08-1024.
- ↑ a b Jo YH, Talmage DA, Role LW (2002). «Nicotinic receptor-mediated effects on appetite and food intake». J Neurobiol 53 (4): 618-32. PMC 2367209. PMID 12436425. doi:10.1002/neu.10147.
- ↑ Klag MJ (1999). Johns Hopkins family health book. New York: HarperCollins. p. 86. ISBN 0-06-270149-5.
- ↑ Farley AC, Hajek P, Lycett D, Aveyard P (2012). «Interventions for preventing weight gain after smoking cessation». En Aveyard, Paul, ed. Cochrane Database Syst Rev 1 (1): CD006219. PMID 22258966. doi:10.1002/14651858.CD006219.pub3.
- ↑ Covey LS, Glassman AH, Stetner F (1997). «Major depression following smoking cessation». Am J Psychiatry 154 (2): 263-5. PMID 9016279.
- ↑ Borrelli B, Bock B, King T, Pinto B, Marcus BH (1996). «The impact of depression on smoking cessation in women». Am J Prev Med 12 (5): 378-87. PMID 8909649.
- ↑ Máirtín S. McDermott, Theresa M. Marteau, Gareth J. Hollands, Matthew Hankins and Paul Aveyard. «Change in anxiety following successful and unsuccessful attempts at smoking cessation: cohort study». BJP.
- ↑ American Cancer Society (31 de enero de 2011). «When smokers quit -- What are the benefits over time?». Consultado el 20 de febrero de 2011.
- ↑ Peto R, Darby S, Deo H, Silcocks P, Whitley E, Doll R (2000). «Smoking, smoking cessation, and lung cancer in the UK since 1950: combination of national statistics with two case-control studies». BMJ 321 (7257): 323-9. PMC 27446. PMID 10926586. doi:10.1136/bmj.321.7257.323.
- ↑ a b Doll R, Peto R, Boreham J, Sutherland I (2004). «Mortality in relation to smoking: 50 years' observations on male British doctors». BMJ 328 (7455): 1519. PMC 437139. PMID 15213107. doi:10.1136/bmj.38142.554479.AE.
- ↑ Anthonisen NR, Skeans MA, Wise RA, Manfreda J, Kanner RE, Connett JE; Lung Health Study Research Group (2005). «The effects of a smoking cessation intervention on 14.5-year mortality: a randomized clinical trial». Annals of Internal Medicine 142 (4): 233-9. PMID 15710956. doi:10.7326/0003-4819-142-4-200502150-00005.
- ↑ «Smoking Cessation Reduces Postoperative Complications». Journalist's Resource.org.
- ↑ Cromwell J, Bartosch WJ, Fiore MC, Hasselblad V, Baker T (1997). «Cost-effectiveness of the clinical practice recommendations in the AHCPR guideline for smoking cessation». JAMA 278 (21): 1759-66. PMID 9388153. doi:10.1001/jama.278.21.1759.
- ↑ Hoogendoorn M, Feenstra TL, Hoogenveen RT, Rutten-van Mölken MP (2010). «Long-term effectiveness and cost-effectiveness of smoking cessation interventions in patients with COPD». Thorax 65 (8): 711-8. PMID 20685746. doi:10.1136/thx.2009.131631.
- ↑ Bauld L, Boyd KA, Briggs AH, Chesterman J, Ferguson J, Judge K, Hiscock R (2011). «One-year outcomes and a cost-effectiveness analysis for smokers accessing group-based and pharmacy-led cessation services». Nicotine Tob Res 13 (2): 135-45. PMID 21196451. doi:10.1093/ntr/ntq222.
- ↑ Schiaffino A, Fernández E, Kunst A, Borrell C, García M, Borràs JM, Mackenbach JP (2007). «Time trends and educational differences in the incidence of quitting smoking in Spain (1965–2000)». Prev Med 45 (2–3): 226-32. PMID 17604832. doi:10.1016/j.ypmed.2007.05.009.
- ↑ Fowkes FJ, Stewart MC, Fowkes FG, Amos A, Price JF (2008). «Scottish smoke-free legislation and trends in smoking cessation». Addiction 103 (11): 1888-95. PMID 19032538. doi:10.1111/j.1360-0443.2008.02350.x.
- ↑ Federico B, Costa G, Ricciardi W, Kunst AE (2009). «Educational inequalities in smoking cessation trends in Italy, 1982–2002». Tob Control 18 (5): 393-8. PMID 19617220. doi:10.1136/tc.2008.029280.
- ↑ Zuo, Xiaoan; Zhao, Halin; Zhao, Xueyong; Guo, Yirui; Yun, Jianying; Wang, Shaokun; Miyasaka, Takafumi (2009). «Cigarette smoking among adults and trends in smoking cessation - United States, 2008». MMWR Morb Mortal Wkly Rep 58 (44): 1227-32. PMID 19910909.
- ↑ Qian J, Cai M, Gao J, Tang S, Xu L, Critchley JA (2010). «Trends in smoking and quitting in China from 1993 to 2003: National Health Service Survey data». Bull World Health Organ 88 (10): 769-76. PMC 2947036. PMID 20931062. doi:10.2471/BLT.09.064709.
- ↑ Error en la cita: Etiqueta
<ref>no válida; no se ha definido el contenido de las referencias llamadasChapman-MacKenzie - ↑ Martin, Anya (13 de mayo de 2010). «What it takes to quit smoking». MarketWatch (Dow Jones). p. 2. Consultado el 14 de mayo de 2010.
